Alternative and complementary medicine as a pathway to care for New Zealand military Veterans experiencing pain and distress.

5 April 2022
Increasingly over the last decade, acupuncture has been successfully used with Veterans internationally and in New Zealand to treat a wide variety of mental health injuries, in conjunction with other complementary and conventional treatment options, as part of a comprehensive, holistic, Veteran-centric clinical package.
An exciting new project is about to start. Headed by Dr David McBride, a team from Otago University, Toi Ohomai Institute of Technology and Acupuncture New Zealand are about to embark on a ground-breaking study looking at the use of acupuncture, action and commitment therapy (ACT) and Rongoa Māori healing for the treatment of New Zealand’s Veterans who are dealing with ongoing distress stemming from their work within the Defence Forces.
Distress is a problem in a significant minority of New Zealand military Veterans. Mobility, carrying out usual activities, and pain or discomfort cause at least some problems for a significant proportion of veterans.
Musculo-skeletal, cognitive and psychophysiological distress are common. An Australian study has shown that it is not uncommon for Veterans to develop chronic diseases such as sleep apnoea, psychological disorders, and cardiovascular conditions. They also demonstrated a range of other risk factors: a high prevalence of obesity, high waist circumference, and harmful alcohol use. They also had poorer physical and mental health. Many Veterans are also lonely and reluctant to access support. Social and geographic isolation are risk factors, as are anxiety and depression.
Battlefield Acupuncture is an auriculotherapy developed by the United States military. 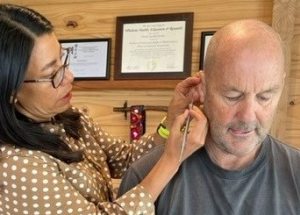
Action and Commitment Therapy (ACT) is a particular form of ‘talking therapy’ which teaches that thoughts and feelings should be accepted and acted upon.
For Māori Veterans, traditional Rongoa Māori healing would be an acceptable treatment, and more effective in improving symptoms of pain and distress than usual approaches to health management.
In Military Medicine, Battlefield Acupuncture has been reported to reduce acute pain, and has become widely adopted for pain management by the United States military. For psychological symptoms, ACT has been shown as a relatively simple approach to reduce distress and to improve sleep through increasing psychological flexibility. Both have been found effective, however acupuncture has been particularly useful for those who have an aversion to talk therapies. For Veterans identifying as Māori, Rongoā Māori, traditional healing, will be available.
The aim of the study is to determine if either Battlefield Acupuncture and ACT, or Rongoa Māori, are more effective in reducing symptoms of pain and distress than ‘usual care,’ - how veterans manage their own symptoms.
 The primary outcome is to determine whether these practices will have greater efficacy than usual care alone in reducing distress.
The primary outcome is to determine whether these practices will have greater efficacy than usual care alone in reducing distress.
The secondary outcome will measure whether pain, disability, sleep quality and symptoms of PTSI will be reduced, and that psychological flexibility will increase.
This will be a funded, nation-wide, multi-centre study.
How to access treatment
Veterans can gain access to the study through their General Practitioner (GP) but initial advice may be sought from New Zealand Veterans Affairs or the RSA District Support Managers. The GPs will then refer the Veteran to the nearest participating acupuncturist and to the study web-site for registration as a potential participant.
For funding purposes, GPs can make an ACC claim to cover the costs of treatment, NZVA Case Managers can authorise treatment for eligible Veterans, RSA District Support Managers can Submit an application for Poppy Funds, and study funding is available for those who do not have other means.
Your nearest RSA District Support Manager: District Support Managers (rsa.org.nz)
Veterans Affairs NZ: Veterans' Affairs (veteransaffairs.mil.nz)
Practitioner ‘Veteran Competency’ training
Decades of experience and research have shown that more effective and longer lasting wellbeing outcomes are more likely if service providers understand how military culture and service may impact Veterans and their families / whanau, and engage with them in a culturally appropriate way.
The Royal NZ Returned and Services Association (RNZRSA) have joined with Acupuncture NZ to develop New Zealand's first 'Veteran Ready' Certification Process that ensures militarily culturally safe acupuncture services for Veterans and their family/whanau.
This is achieved by developing a treatment provider’s understanding of what is important to a Veteran and their family/whanau, how military service may influence Veteran behaviour and how this may impact on accessing, responding to, or engaging in acupuncture services.
Acupuncturists routinely identify patterns of lifestyle, sleep patterns, movements, thought patterns and emotions. Practitioners involved in the study will undergo specific training in the use of Battlefield acupuncture, as organised by Acupuncture NZ. They will also complete training in the ACT techniques. Additionally they are required to complete specific online modules as identified by the RSA from the PsychArmor website.
Once an individual provider has completed a broad-based education package, provided by international and domestic experts, and provided evidence of meeting agreed clinical protocols, they are certified as 'Veteran Ready' by the RNZRSA and AcupunctureNZ.
Those practitioners who have completed the Veteran Competency training will be readily identifiable through the Veterans “Find a Practitioner” facility on this website.
Significance
He Ara Oranga, the Report of the Government Inquiry into Mental Health and Addiction, highlighted the increasing demand for mental health services, the rising use of pharmacological treatment, and inequities in access to psychological services. Using ‘talking therapies’ is seen as a viable way forward, but faces the barrier of the limited number of psychologists available to treat the more seriously affected patients. The alternative suggestion was to involve counsellors and social workers in treatment at ‘the milder end of the spectrum.’ Acupuncturists and Rongoa Māori practitioners are skilled in ‘talking through’ problems, so this proposal addresses a pathway to care for Military Veterans with pain and distress, integrating a ‘Veteran acceptable’ complementary and alternative medicine (CAM) approach to address their needs. There is no reason why the approach should not be successful in similar groups: First Responders and Public Safety Personnel, or indeed the general public.
